By NAOMI GOLDMAN
By NAOMI GOLDMAN
Images courtesy of Dr. “Skip” Rizzo and the USC Institute for Creative Technologies.

Extended Reality via AI, VR and AR technologies pioneered by Albert “Skip” Rizzo, Ph.D. has revolutionized the delivery of patient-centered mental health care, offering innovative, engaging and effective therapies that are changing the treatment landscape for medical professionals and relief-seekers.
As a clinical psychologist and Director of the University of Southern California Institute for Creative Technologies (ICT) Medical VR Lab and Research Professor at the USC’s Department of Psychiatry and School of Gerontology, Dr. Rizzo has spent more than three decades at the forefront of clinical virtual reality, conducting research on the design, development and evaluation of VR systems across the domains of psychological, cognitive and motor functioning in healthy and clinical populations. A trailblazer at the intersection of clinical psychology, neuroscience and immersive technology, his work has focused on PTSD, Autism, ADHD, Alzheimer’s disease, stroke, psychedelic therapy, suicide prevention and other clinical conditions. Dr. Rizzo is best known for his empirically validated use of VR in the treatment of combat and sexual trauma-related PTSD.
In this one-on-one with VFX Voice, Dr. Rizzo shares his current views on the dynamic field of VR-based therapy, the deepening of his trauma-based work, and harnessing AI and digital humans.
VFX Voice: In the years since you last discussed VR/AR/XR and their use as therapeutic tools with VFX Voice in 2017, how has the field evolved?
Dr. Rizzo: The whole field of clinical applications using VR/XR/AR has evolved dramatically in several ways. First, the technology has caught up with the vision, including products developed by Meta, PICO and HTC that have surpassed what we could have dreamed of – low-cost, high-fidelity headsets and tech for developing these experiences. So, we can really deliver at scale for clinical purposes.
Second, the science has advanced to the point that we can confidently say that when applied thoughtfully within a proper clinical perspective, these virtual applications make a difference for people in a scientifically valid way. We have data that confirms that these virtual approaches are as good as, or not inferior to, traditional methods, and are actually more appealing, so people will do more. And since everything is measured in a VR environment, we have an ongoing pipeline of data to continually feed back in and evolve the programs and the user experience.
Third, companies are taking academic findings and turning them into products. While that is happening at an accelerated rate, it’s not mainstream yet. As new programs are developed, it’s difficult to break into the medical field, and there’s a learning curve on what programs work for what headset. We need a convergence that brings it all together – a consumer reports-type inventory for both clinicians and lay people to find the best programs and ratings. Folding in virtual humans and virtual environments is the next runway.
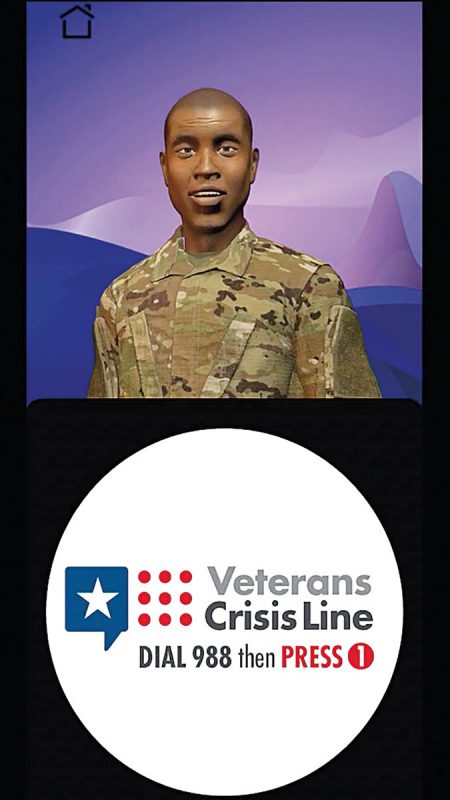
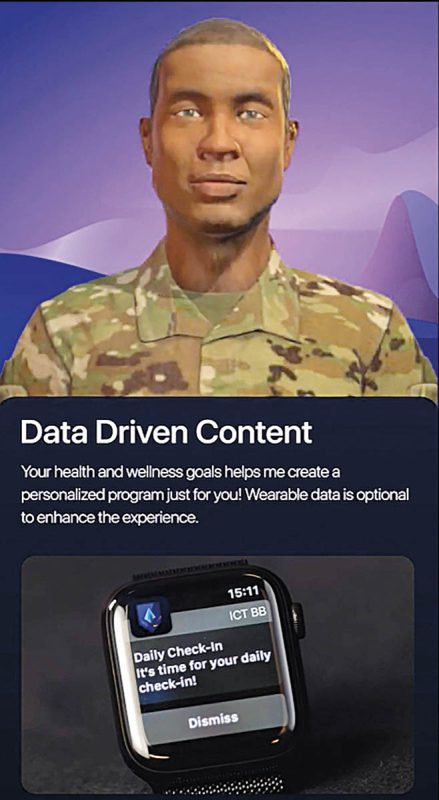
VFXV: On that note, your work with virtual humans and support for military veterans has converged with the creation of Battle Buddy, an AI-driven mobile health (mHealth) application tailored exclusively for veterans and developed in response to the U.S. Department of Veterans Affairs’ Mission Daybreak Challenge to end the epidemic of veteran suicide. Walk us through this program.
Dr. Rizzo: Consider Battle Buddy an ‘in your pocket support agent.’ A virtual human that can interact with users on health and wellness content, as a springboard to real-world support networks, to be a companion for conversation or to play games. In the event of a suicidal crisis, Battle Buddy’s primary focus shifts to guiding veterans through their personalized safety plan. We have incorporated deep content from the Veterans Administration – from questions about the G.I. Bill to finding an apartment to relationship advice – to be that supportive bridge, especially for new veterans. In that first year of transition from military to veteran status, when the structure they have been accustomed to falls away, the suicide rates double. Battle Buddy was designed specifically to address the crisis of veteran suicide and be a companion, and sometimes a lifeline. This module is still in development, and through our partnership with Sidekick [an Augmented Human Intelligence platform that empowers subject matter experts to scale their knowledge through secure, expert-guided AI agents], it has enormous potential to address this crisis.



VFXV: You have envisioned a multitude of applications based on the Battle Buddy model. What are some other populations you’re exploring that could be served by a virtual human companion?
Dr. Rizzo: I’m very interested in maternal health care and disparities. So, the idea is to build out a Birthing Buddy – testing this same model. The user can make an AI character and set up the program to be their partner, remind them of doctor’s visits, offer wellness support, have access to detailed resources and data, and engage in dialogue. While using it, the AI software agent is getting to know the mother-to-be’s health and mental health, and after the baby is born – because the relationship and trust are already established – it can be there to support the mother through post-partum depression and any issues. It can harken back to prior conversations and offer a voice of support with no shame. On the issue of should AI be a substitute for real-life therapists – let’s say not replace them. But some people may not seek help for myriad reasons – from lack of resources to shame of stigma – and this is where AI can fill the gap and be agents of change.
VFXV: Your groundbreaking work on Bravemind, a virtual reality exposure therapy for treating post-traumatic stress disorder in veterans, has been a center point of your trauma-related work. How has Bravemind expanded its scope and applications?
Dr. Rizzo: Our combat-related work with veterans who served in Iraq and Afghanistan has continued, and we have now extended the range of traumatic experiences to include sexual assault survivors within a military context. We integrated VR contexts, putting people into these experiences in the field and at U.S. bases. The model was built out, tested and found effective, so now it is a full-fledged tool for both civilian and military sexual trauma.
Along the way, we started working with people in Ukraine to build a program addressing the civilian and combat experience and the great need for support. USC donated the software code base to a developer in Ukraine, and we built a program with several experiences – a wartime scene in a wooded area with trenches and drones; a city scene; and a country village scene taken over by force – where people can walk around destroyed buildings, experience tanks and Russian soldiers on patrol, or hide out in a house as soldiers approach. We also created a metaverse social gathering place for refugees, where people can occupy an avatar and interact in a shared social support experience to talk about grief, loss and hope. A lot of love went into to building this, and we expect the first open clinical trial by the end of 2025.
We are developing a similar process in Israel in partnership with clinicians at Ben-Gurion University in Israel. This model to treat trauma includes Gaza-like war scenes, and experiences of Hamas missiles flying into homes and kibbutz communities – it is an apolitical tool, working on capturing the full spectrum of the lived experience on the ground. This model takes a different clinical approach – not just exposure to re-process the experience, but a means to go into a space that looks like your wrecked home, and allow the user to visit and clean it up as a means to work through the trauma.
VFXV: How will these VR tools developed for people in Ukraine and Israel be available?
Dr. Rizzo: All my work has a clinician component. In the Ukraine model, the therapy is administered with a clinician, which can be remote; it’s not a self-help model. This is hard medicine for hard problems, in going back to the scene of trauma to confront and process emotional memories in a safe place – even conceptually. Going through the emotional activation with the support and very active engagement of a clinician is key; as someone talks about their story, the clinician can adjust the VR scene to align with the evolving narrative and enhance the realism and effectiveness of the therapy. In Ukraine, the therapy will ultimately be delivered through the International Institute of Postgraduate Education in Kyiv, a psychological training institute with 160-plus clinicians.
VFXV: Using VR to support people with autism spectrum disorder is another focus area of your work. How has this work grown and expanded?
Dr. Rizzo: We developed VITA (Vocational Interview Training Agents) to help people on the autism spectrum who are high functioning and skilled, but have issues with social interaction, to help them succeed in job interviews. We built virtual human characters that reflect different demographics and can pop them into different job contexts [office, restaurant, warehouse] – in total, six characters, seven work contexts and three levels of provocativeness – a nice, neutral or nasty interviewer – allowing for many scenarios. This can be done on a headset, but mostly we’re delivering this role-play on a laptop or big-screen TV, so the user can sit with a vocational counselor and keep practicing, combining skills training and an experiential approach to confronting fear. Through a partnership with the Dan Marino Foundation in Florida, this 10-year program has been distributed to more than 170 schools, special need programs and clinicians. We made the application generic enough where we only had to change some lines to make it appropriate for veterans or other disadvantaged populations with challenges to overcome in the job market. And we’re now working to integrate more AI into the program components to expand its capacity.
VFXV: What are some of the hot button ethical issues and implications related to VR/AR/XR and treating mental health?
Dr. Rizzo: The big debate is centered on two issues. First, when it comes to bringing AI into the mix of clinical care – and replacing clinicians with virtual therapists on using AI support agents – should we be doing it in the first place? In the ideal world, all humans would be optimal. But looking at the latest World Health Organization’s stats that estimate 1 billion people have a mental health issue and two-thirds will never see the inside of a therapy office – because of access, resources or stigma – conversion to AI can play a vital role in meeting unaddressed needs. Research shows that some patients are more likely to disclose personal information to an AI character as they have less worry about being judged or making an impression. And it is always a motive that if you have a serious problem you understand with AI interaction, we will try and guide you to talk with a real person offering genuine empathy and counsel.
The other issue is trust. We don’t fully know how AI agents actually work and they sometimes hallucinate and give bad information, notably in two cases where the AI agent helped users develop and execute suicide plans. Now, ChatGPT has safeguards if you start talking about suicide. And when it comes to our apps like Battle Buddy, all of the content delivered to the veteran is researched and vetted, and the program has been red team-tested.
As we navigate these important considerations and manifest our responsibilities as researchers and clinicians, it is clear that innovative XR deployments are scaling our ability to deliver patient-centered care in ways that transcend traditional treatment.


